Gordie Howe’s Stem Cells Treatments Support a Growing Appeal for These Therapies Among Athletes and Baby Boomers
In October, 2014, legendary hockey player Gordie Howe, then 86, was on death’s door after suffering a debilitating acute hemorrhagic, left thalamus stroke. Upon returning home from the hospital, Howe needed someone to lift him from his bed to a wheelchair and back. He couldn’t remember the names of his four children, Marty, Mark, Cathy, and Murray, and his condition continued to grow worse in subsequent weeks. According to an article in New York Magazine, when Mark took his father to get an epidural to relieve his back pain, the attending physician took one look at Gordie and asked Mark if it might be better to just let his father go. On the rare occasion when Gordie did manage to speak, he would tell his children, “Just take me out back and shoot me.”
The man for whom the term “hat trick” was coined, Howe retired from hockey at age 52 after four decades of professional play, having scored more goals than any other NHL player. But over the past 10 years, his health declined dramatically—heart disease, dementia, and spinal stenosis—despite his family’s and physician’s best efforts to find medical solutions. After his stroke, Keith Olbermann aired a preemptive obituary on ESPN. The family made funeral plans. Murray, his youngest son, wrote a eulogy.
Experimental stem cell treatment
Around Thanksgiving, 2015, Howe’s family learned about an experimental stem cell treatment that could save his life. The plan was to inject up to 100 million neural stem cells into his spinal column in the hopes that the stem cells would migrate to his brain and help his body repair itself. Howe could improve within 24 hours, and receive the treatment anytime—just not in the United States. The procedure wasn’t FDA-approved, and Howe would have to receive the treatment at a clinic in Tijuana.
Howe’s son Murray, a radiologist, looked into the treatment and thought it was promising. The real concern was transporting the immobile Howe to Mexico. Daughter Cathy worried that he might die during the treatment, but Mark responded bluntly: “If he does die, what’s the difference? He’s going to be gone soon no matter what.”
While the family weighed the stem cell treatment idea, Howe was admitted to the hospital with severe dehydration, caused by his unwillingness to swallow. When he returned home, he still had no use of his right side, and the family assumed he would never walk again. The Howe children decided to give the stem cell treatments a try.
Two days later, the Howes flew their Dad to San Diego. In the air, Gordie grew agitated and got the attention of a flight attendant, who spent 10 minutes kneeling by his seat trying to understand something he wanted to tell her. Due to his profound memory loss, Howe didn’t know he had suffered a stroke, why he was on a plane, or where he was going. But he remembered one thing, which he managed to whisper to the fight attendant: “I was a pro hockey player.”
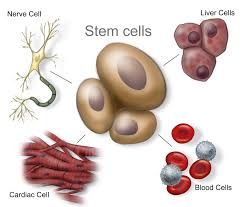
The next morning, Marty and Murray drove with their father across the border to Clínica Santa Clarita, where Gordie bent over a table to expose his lower back so that a needle could be inserted into his spinal canal to inject the stem cells. Howe was given two types of stem cells – neural stem cells and mesenchymal stem cells. The second type, derived from bone marrow, has anti-inflammatory properties and secretes chemicals that promote healing.
The procedure then required Howe to lie prone for eight hours. After the eight hours passed, Gordie told Murray he needed to use the bathroom and that he intended to walk there in order to do so. Since the stroke, Gordie had only managed to walk one time—10 steps, with a walker. Murray reminded his Dad that he couldn’t walk.
Recovery milestone after stem cell treatment
Howe stood up, and with Murray’s support, walked for the first time in more than a month—to the bathroom. This milestone became an oft-repeated story among the Howe family, and Gordie’s revival became an irresistible story for the sports pages. Back home, Gordie returned to something resembling the normal life of an 86-year-old. He pushed the grocery cart, helped with the dishes, and could go fishing so long as one of his sons reminded him that a tug on the line meant he needed to start reeling. The family released a video of Gordie standing stationary, firing a puck, five-hole, past his 8-year-old great-grandson. Keith Olbermann apologized for his premature obituary.
Howe’s children now had to figure out how to share his apparent recovery—a debate that proved just as contentious as their decision to fly him to Mexico for the treatment in the first place—with the world. Both Marty and Mark had played in the NHL alongside their father, but now Murray, the doctor, was giving interviews in his hospital scrubs, endorsing his father’s place in medical “miracle” history. He began referring to the stem-cell treatment as the “Gordie Howe Protocol,” and said that his Toledo-based hospital was looking into conducting an FDA-approved study of the procedure. In one interview, Murray Howe stated that “stem cells are the most promising thing in medicine since the discovery of antibiotics.”
As the story spread, the medical community started to question just how miraculous Howe’s recovery had been.
“Companies selling these products are preying on desperate and vulnerable people and exploiting their hope, much like snake-oil salesmen have done throughout most of human history,” wrote Judy Illes and Fabio Rossi, stem-cell experts at the University of British Columbia, in the Vancouver Sun. Even advocates pointed out that, though the field holds great promise, no reputable studies have shown that such a procedure should work.
And yet, for the children of ailing parents, such skepticism doesn’t matter. Murray’s response to one skeptic was, “What would you do for your father?”
Gordie Howe’s therapy would cost an average patient about $30,000.
Athletes, whether playing or retired, have a special need for the regenerative capacity that stem cells are believed to provide. Athletes break bones, strain ligaments, bash knees and wear out cartilage. If stem cells’ restorative capability is proven, they could be considered the latest form of sports medicine.
Since Howe’s treatment in late 2014, two other athletic legends have received stem cell treatments—former quarterbacks Bart Starr and John Brodie. And the rest of the population, particularly aging baby boomers, isn’t far behind.
 Still, while acceptance of stem cell therapy has grown, so have controversies surrounding its use. While clinical trials authorized by the U.S. Food and Drug Administration are rapidly expanding in the U.S., so are treatments outside the regulated system. Patients are going to stem cell clinics in other countries that approve stem cell therapies.
Still, while acceptance of stem cell therapy has grown, so have controversies surrounding its use. While clinical trials authorized by the U.S. Food and Drug Administration are rapidly expanding in the U.S., so are treatments outside the regulated system. Patients are going to stem cell clinics in other countries that approve stem cell therapies.
For its part, the FDA is drafting guidelines, although the U.S. and Canada still trail other countries in approving stem cell treatments.
Last year, the FDA issued draft guidelines to clarify what types of human cell therapy it regulates. The short answer: Most of them, with “limited exceptions,” according to an FDA email sent in response to questions from The San Diego Union-Tribune. These exceptions include cells or tissues that are “minimally manipulated,” not given with any other product and perform the same function in the donor as in the recipient.
All other stem cell therapies are seen as involving human cells, tissues and cellular and tissue-based products – also known as HCT/Ps – regulated by the FDA’s Center for Biologics Evaluation and Research.
“We understand that determining the appropriate regulatory path for HCT/Ps can be challenging, and the FDA is working diligently to develop guidance to help sponsors and physicians understand how to apply federal regulations to this complex and emerging field,” the agency said.
In January 2015, University of California, Davis stem cell researcher and blogger Paul Knoepfler estimated that more than 100 unauthorized stem cell clinics were operating in the United States. Later that year, he increased that estimate to up to 200.
Then on May 6, he wrote in his blog: “We are seeing a flood of professional athletes getting stem cell treatments in the past few years.”
Athletes and others who want these treatments bristle at what they call cumbersome, time-consuming regulations in the U.S. The situation can be urgent for seriously ill patients.
While it hasn’t been proven that the stem cells enabled his recovery, by all indications Gordie Howe’s health has improved significantly since receiving stem cell treatments. In November, 2015, Murray Howe said that his father’s physicians in the U.S. recommended hospice care in the weeks after the stroke, and the family was told he wouldn’t last more than two or three weeks,
“Then, suddenly, he is raking and sweeping and goofing around in the back yard,” Murray said.
###
###
Sources: The San Diego Union-Tribune, New York Magazine

 In the study, scientists investigated the role of the
In the study, scientists investigated the role of the 
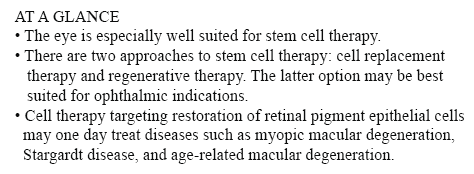 cone cells, which now can be produced in high quantities.
cone cells, which now can be produced in high quantities.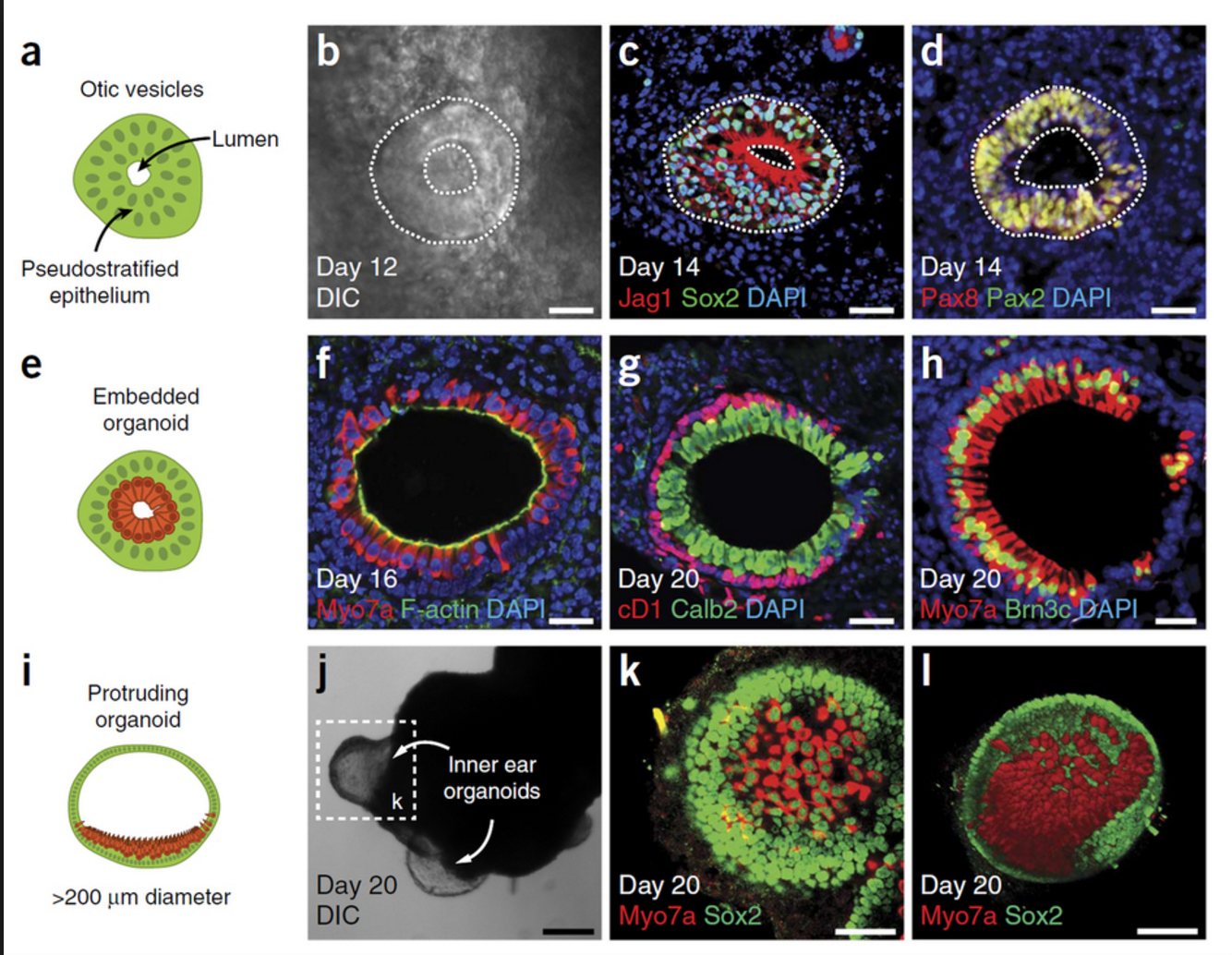 “The goal isn’t just to make the closest thing next to a real retina, but also to possibly harness the flexibility of the system to create more diverse ways of studying retina tissue,” says senior author Mike Karl, of the German Center for Neurodegenerative Diseases (DZNE) and part of the Center for Regenerative Therapies (CRTD) at Technische Universität Dresden.
“The goal isn’t just to make the closest thing next to a real retina, but also to possibly harness the flexibility of the system to create more diverse ways of studying retina tissue,” says senior author Mike Karl, of the German Center for Neurodegenerative Diseases (DZNE) and part of the Center for Regenerative Therapies (CRTD) at Technische Universität Dresden.

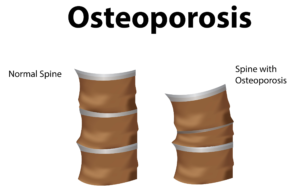
 porosis, there is a reduction in the inner structure of the bone. The bone becomes thinner and less dense, and it can no longer function properly.
porosis, there is a reduction in the inner structure of the bone. The bone becomes thinner and less dense, and it can no longer function properly.
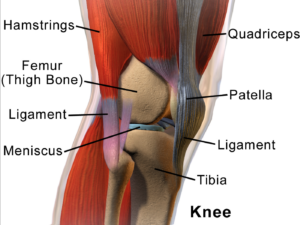
 n considered as an ideal candidate for cell therapy as it is a relatively simple tissue, composed of one cell type, chondrocytes, and does not have a substantial blood-supply network. Of particular interest to researchers is repair of cartilage tissue in the knee, also called the meniscus of the knee. The meniscus is responsible for distributing the body’s weight at the knee joint when there is movement between the upper and lower leg. Only one third of meniscus cartilage has a blood supply, and as the blood supply allows healing factors and stem cells attached to the blood vessels (called perivascular stem cells) to access the damaged site, the meniscus’s natural lack of blood supply impairs healing of this tissue. Damage to this tissue is common in athletes, and is the target for surgery in 60 percent of patients undergoing knee operations, which usually involves the partial or complete removal of the meniscus, which can lead to long-term cartilage degeneration and
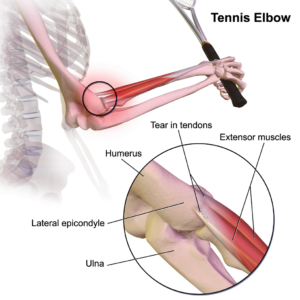
n considered as an ideal candidate for cell therapy as it is a relatively simple tissue, composed of one cell type, chondrocytes, and does not have a substantial blood-supply network. Of particular interest to researchers is repair of cartilage tissue in the knee, also called the meniscus of the knee. The meniscus is responsible for distributing the body’s weight at the knee joint when there is movement between the upper and lower leg. Only one third of meniscus cartilage has a blood supply, and as the blood supply allows healing factors and stem cells attached to the blood vessels (called perivascular stem cells) to access the damaged site, the meniscus’s natural lack of blood supply impairs healing of this tissue. Damage to this tissue is common in athletes, and is the target for surgery in 60 percent of patients undergoing knee operations, which usually involves the partial or complete removal of the meniscus, which can lead to long-term cartilage degeneration and  muscles to bones. Tendons become strained and damaged through repetitive use, making tendinopathy a common injury among athletes. Tendinopathy has been linked to 30 percent of all running-related injuries, and up to 40 percent of tennis players suffer from some form of elbow tendinopathy or “tennis elbow.” Damage occurs to the collagen fibers that make up the tendon, and this damage is repaired by the body through a process of inflammation and production of new fibers that fuse together with the undamaged tissue. However, this natural healing process can take up to a year to resolve, and results in the formation of a scar on the tendon tissue, reducing the tendon’s natural elasticity, decreasing the amount of energy the tissue can store and resulting in a weakening of tendon.
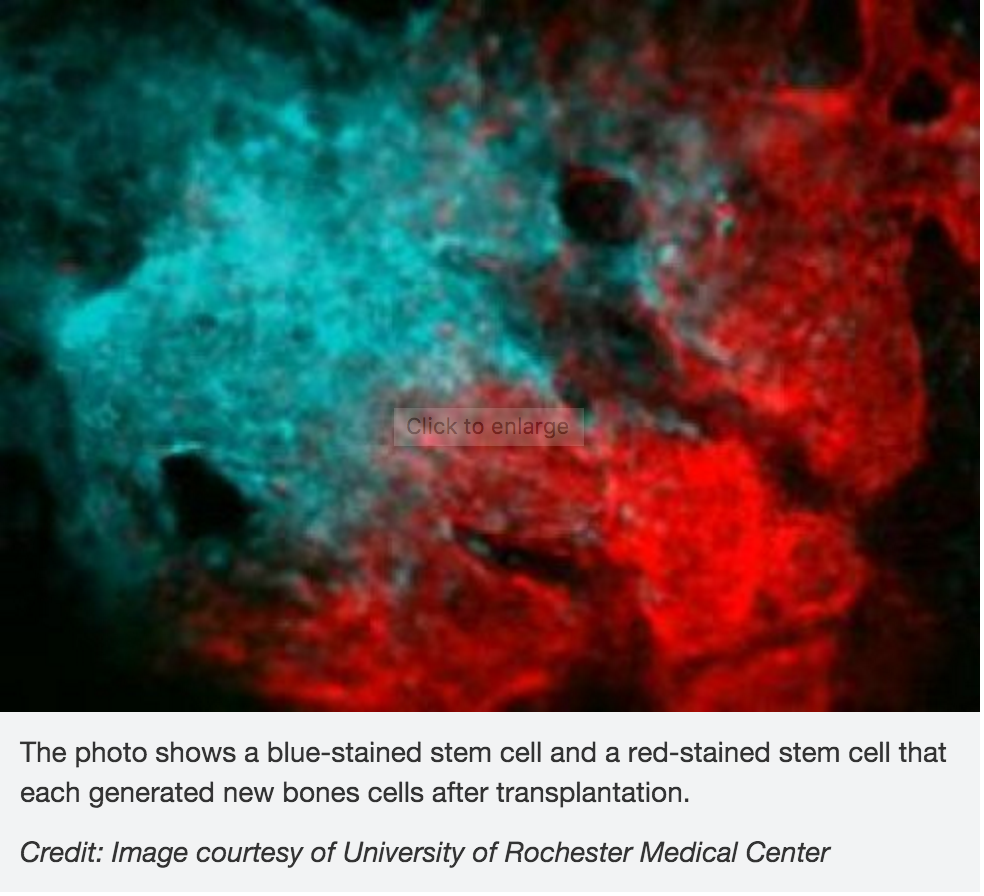
muscles to bones. Tendons become strained and damaged through repetitive use, making tendinopathy a common injury among athletes. Tendinopathy has been linked to 30 percent of all running-related injuries, and up to 40 percent of tennis players suffer from some form of elbow tendinopathy or “tennis elbow.” Damage occurs to the collagen fibers that make up the tendon, and this damage is repaired by the body through a process of inflammation and production of new fibers that fuse together with the undamaged tissue. However, this natural healing process can take up to a year to resolve, and results in the formation of a scar on the tendon tissue, reducing the tendon’s natural elasticity, decreasing the amount of energy the tissue can store and resulting in a weakening of tendon. Bones are unique in that they have the ability to regenerate throughout life. Upon injury, such as a fracture, a series of events occur to initiate healing of the damaged bone. Initially there is inflammation at the site of injury, and a large number of signals are sent out. These signals attract MSCs, which begin to divide and increase their numbers. The MSCs then change into either chondrocytes, the cells responsible for making a type of cartilage scaffold, or osteoblasts, the cells that deposit the proteins and minerals that comprise the hard bone on to the cartilage. Finally these new structures are altered to restore shape and function to the repaired bone. A number of studies carried out in animals have demonstrated that direct injection or infusing the blood with MSCs can help heal fractures that previously failed to heal naturally. However, as was the case with tendinopathy, it is not yet clear if these external MSCs work by generating more bone-producing cells or through their ability to reduce inflammation and encourage restoration of the blood supply to injured bone, or both.
Bones are unique in that they have the ability to regenerate throughout life. Upon injury, such as a fracture, a series of events occur to initiate healing of the damaged bone. Initially there is inflammation at the site of injury, and a large number of signals are sent out. These signals attract MSCs, which begin to divide and increase their numbers. The MSCs then change into either chondrocytes, the cells responsible for making a type of cartilage scaffold, or osteoblasts, the cells that deposit the proteins and minerals that comprise the hard bone on to the cartilage. Finally these new structures are altered to restore shape and function to the repaired bone. A number of studies carried out in animals have demonstrated that direct injection or infusing the blood with MSCs can help heal fractures that previously failed to heal naturally. However, as was the case with tendinopathy, it is not yet clear if these external MSCs work by generating more bone-producing cells or through their ability to reduce inflammation and encourage restoration of the blood supply to injured bone, or both. dergo cell death and patients develop dementia. Researchers have attempted a number of strategies to investigate treatments of this disease in mice, including introducing neural stem cells that could produce healthy neurons. While some of these experiments have demonstrated positive, if limited, effects, to date there are no stem cell treatments available for Alzheimer’s Disease.
dergo cell death and patients develop dementia. Researchers have attempted a number of strategies to investigate treatments of this disease in mice, including introducing neural stem cells that could produce healthy neurons. While some of these experiments have demonstrated positive, if limited, effects, to date there are no stem cell treatments available for Alzheimer’s Disease.
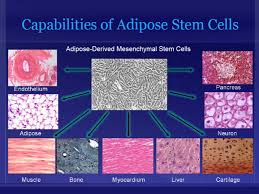
 themselves, they can divide and form bone, cartilage, muscle, and adipose (fat) stem cells when cultured under certain conditions. MSCs are attractive to researchers and clinicians since they can be readily isolated from a variety of patient tissues, including fat. Once harvested and, if necessary, elevated to high numbers in culture, MSCs can be re-introduced to the patient from whom they were harvested, eliminating any risk of immune-rejection. In response to injury, MSCs produce proteins that appear to alter the surrounding environment and promote healing and tissue regeneration, such as anti-inflammatory factors, angiogenic factors (which promote the growth of new blood vessels) and other factors that stimulate local, tissue-specific stem cells.
themselves, they can divide and form bone, cartilage, muscle, and adipose (fat) stem cells when cultured under certain conditions. MSCs are attractive to researchers and clinicians since they can be readily isolated from a variety of patient tissues, including fat. Once harvested and, if necessary, elevated to high numbers in culture, MSCs can be re-introduced to the patient from whom they were harvested, eliminating any risk of immune-rejection. In response to injury, MSCs produce proteins that appear to alter the surrounding environment and promote healing and tissue regeneration, such as anti-inflammatory factors, angiogenic factors (which promote the growth of new blood vessels) and other factors that stimulate local, tissue-specific stem cells.